Vishwajeet Modi1, MCG Karunanayake2.
1Royal Perth Hospital, Perth, Australia,
2Armadale Health Service, Perth, Australia.
ADDRESS FOR CORRESPONDENCE
Vishwajeet Modi, 35 Parkway Gardens, Parmelia, WA 6167, Australia.
Email: vishwajeet.modi@gmail.com | | Abstract | Aim:
Accurate newborn length measurement is essential for growth trajectory assessment. The gold-standard is the standardised supine-length board (Infantometer).1 The survey aims to evaluate the awareness and usage of the Infantometer among midwives and nurses at a metropolitan Australian hospital, identify barriers to its use, assess willingness to undergo training and recommend strategies for implementing the Infantometer as a routine practice.
Methods:
A voluntary e-survey was distributed via email to midwives and nurses at the hospital working in the labour, special care nursery, post-natal and paediatric wards.
Results:
Out of 81 respondents, 82.7% used the Tape-measure method, with only 34.3% aware of the Infantometer. Nurses were more likely to use the Infantometer than midwives (59.9% vs 5.1%, p<0.001). There was significant variability in measurement tools used across different wards (p<0.001). A majority (92.6%) supported the introduction of the Infantometer at the hospital. Concerns about the Infantometer included practicality, storage, maintenance and potential discomfort for infants.
Conclusion:
The Tape-measure method is commonly used due to its speed and accessibility, despite the Infantometer being more accurate. Training programs focused on midwives and staff in the labour, special care nursery and post-natal wards are recommended to improve awareness and usage of the Infantometer. Addressing concerns about the Infantometer and providing comprehensive training can facilitate its adoption and improve the accuracy of newborn length measurements. | | | | Keywords | | Survey, Infantometer, Length measurement. | | | | Introduction | What is already known on this topic:
1. The Tape-measure method is an inaccurate method of measuring neonatal length, the gold-standard is the standardised supine-length board (Infantometer).
2. Accurate newborn length measurement is crucial as it is a primary indicator of neonatal nutrition and serves as a baseline for future growth trajectories.
3. Accurate measurements are essential for utilizing standard growth curves, which guide treatment decisions.
What this study adds:
1. This study showcases the variability in newborn length measurement technique at an Australian metropolitan hospital.
2. Nurses use the Infantometer more than midwives. However, a significant portion of staff that use the Tape-measure method were not aware of the Infantometer, this was seen across both nurses and midwives. Despite this, there’s a high willingness among both professions to learn more about the Infantometer.
3. The survey reveals barriers present to the adaptation of the Infantometer (gold-standard) as routine practice for newborn length measurement and recommends strategies for implementing the Infantometer.
An accurate newborn length measurement is important as it is a primary indicator of neonatal nutrition along with weight. It serves as a baseline for which future growth trajectories are based on. Standard growth curves guide treatment decisions, thus it is essential to have accurate measurements. The Infantometer is the gold-standard for newborn length measurement.1 Although popular, the Tape-measure method results in inaccuracies in measurement which has implications for potentially misguided clinical care.2,3
Unlike birthweight and occipitofrontal circumference, it is not necessary to check length immediately after birth. It can be done before discharge or within 48 hours. Currently at this hospital, there are variations in the methods used to measure newborn length between staff members and across wards. The two methods used at the hospital include: the Tape-measure method and the standardised supine-length board (Infantometer). This survey aims to:
1. Evaluate current usage and awareness of the Infantometer.
2. Identify if there is any difference in awareness and usage of the Infantometer between midwives and nurses working with paediatric patients.
3. Identify barriers preventing the use of the Infantometer.
4. Gauge midwives and nurses’ willingness to train in using the Infantometer.
5. Make recommendations to aid implementation of the Infantometer as routine practice.
| | | | Methods | This was a voluntary, cross-sectional e-survey conducted using the REDCap registry. The survey was designed to take approximately 5 minutes to complete and did not collect personal identifying data (Appendix #1 includes the full list of survey questions). The survey followed the "Checklist for Reporting of Survey Studies" guideline, but no pretesting or piloting was conducted, which is noted as a limitation of the study.
The survey was e-mailed on the 23/08/2023 to Midwives and Nurses at the hospital working on the labour, special care nursery, post-natal and paediatric wards. The email list was sourced from the nursing and midwifery manager who had a list of all the eligible working nurses and midwives at the hospital. The survey was open for 2 weeks from 23/08/2023 to 06/09/2023. Responses that were partially completed were excluded from the study, n=2. All responses to the survey questions were recorded and used to compare outcomes across staff (nurses vs midwives) and wards (labour, special care nursery, post-natal, paediatric).
The survey questions were developed to fulfill the objectives of the study and to cover the following outcomes of interest:
- Number of respondents utilising Infantometer vs Tape-measure method.
Number of respondents using the Tape-measure method who’re aware of the Infantometer.
- Number of respondents who prefer Infantometer vs Tape-measure method and their reason for preference.
- Number of respondents happy to implement Infantometer as routine practice on their ward or if unhappy, their reason for it.
Please see Appendix #1 for full list of questions.
Statistical tests were performed using SPSS statistics program and the Pearson Chi-Square test was used to compare nominal data, with level of significant set to 0.05.
To reduce social desirability bias, participants were informed at the beginning of the survey that their response will be anonymous.
Ethical approval was not needed for this study. | | | | Results | There were 83 survey responses, 2 of which were partially completed and hence excluded from the analysis. Table 1 summarises the demographic of the survey respondents.
The majority of respondents were midwives (n=62), while the remaining were nurses (n=19), as described in Table 1.
Table 1. Demographic information of the survey participants.
| |
Which area do you predominantly work in? |
|
| Labour ward |
Special care nursery |
Post-natal ward |
Paediatric |
Other - specify |
Total |
| How do you identify yourself? |
Nurse |
1 |
8 |
1 |
8 |
1 |
19 |
| Midwife |
34 |
0 |
17 |
0 |
11 |
62 |
| Total |
|
35 |
8 |
18 |
8 |
12 |
81 |
Overall, 82.7% (95%CI: 0.7270, 0.9022) of the survey respondents used the Tape-measure method (n=67), whilst 17.3% (n=14) used the Infantometer. When comparing usage by role, nurses were significantly more likely to use the Infantometer (57.9%, 95% CI: 0.3350, 0.7975) compared to midwives (5.1%, 95% CI: 0.0101, 0.1350) (p<0.001).
There was also a significant difference seen amongst survey respondents across different wards as seen in Table 2. A notable observation being that 100% (one-sided 97.5%CI: 0.6306, 1.0000) of nurses on the paediatric ward utilised the Infantometer for newborn length measurement, with accuracy cited as the reason for their preference of the tool.
Table 2. Distribution of newborn length practice across different wards.
| |
% Tape-measure method |
% Infantometer method |
| Labour ward |
97.1 |
2.9 |
| Special care nursery |
75.0 |
25.0 |
| Post-natal ward |
88.9 |
11.1 |
| Paediatric |
0 |
100.0 |
(p<0.001)
Out of all the 67 survey respondents that use the Tape-measure method, 34.3% (95%CI: 0.2315.1, 0.4694) were aware of the Infantometer. There was no statistically significant difference between both nurses and midwives, 50.0% of nurses (95%CI: 0.1570, 0.8430) compared with 32.2% (95%CI: 0.2062, 0.4564) of midwives being aware of the Infantometer (p=0.320).
Of the respondents who were unaware of the Infantometer (n=44), 100% (one-sided 97.5%CI: 0.9196, 1.000) responded ‘YES’ to learning how to use the Infantometer.
The survey also explored the frequency of use of the Infantometer in comparison to the Tape-measure method. Participants indicated their usage on a sliding scale ranging from 0% (never) to 100% (always), with increments of 25%. Amongst the respondents who utilized the Infantometer (n=14), the mean usage was 76.8%. Conversely, those who used the Tape-measure method, but were aware of the Infantometer (n=23), had a mean usage of 4.4%.
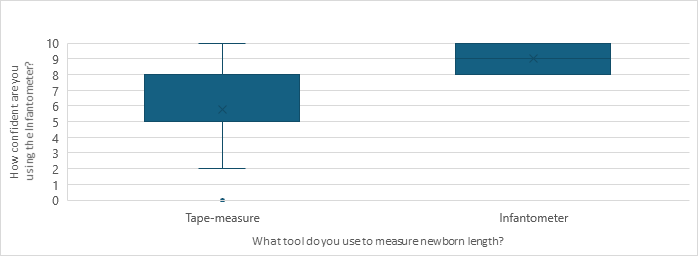
Participants were also queried about their confidence in using the Infantometer, rating it on a scale of 0-10 in increments of 1, where 0 referred to “not at all confident” and 10 meant “very confident.” The participant group using the Infantometer (n=14) had an Interquartile Range (IQR) of 8-10. Meanwhile, those who used the Tape-measure method, but were aware of the Infantometer (n=23), had an IQR of 5-8. Figure 1, a Box-and-Whisker plot, provides a summary of this data.
Figure 1. Infantometer-use confidence between Tape-measure method vs Infantometer users.
In addition to surveying participants about which method of length measurement they used, those aware of both methods were also asked which method they preferred. This was done to draw a comparison between the two and to analyse if there was a discrepancy between their preferred tool versus the tool they use in actual practice.
Of the participants who were aware of both tools, 30.4% (95%CI: 0.1321, 0.5292) of the respondents who use the Tape-measure method, expressed a preference for the Infantometer over the Tape-measure method. On the other hand, amongst the users of the Infantometer, 7.1% (95%CI: 0.0018, 0.3387) indicated a preference for the Tape-measure method over the Infantometer.
Tool-preference was found to be similar between midwives and nurses, 59.09% (95%CI: 0.3635, 0.7929) of midwives preferred the Tape-measure method compared with 73.3% (95%CI: 0.4490, 0.9221) of nurses. This was a statistically insignificant difference between the two groups (p=0.052).
The majority of survey respondents cited speed, ease of use and accessibility as their reasons for preference of the Tape-measure method, as seen in Table 3. On the other hand, the primary reason for favouring the Infantometer was its accuracy. Some survey participants also mentioned additional reasons for their preference of the Tape-measure method over the Infantometer. These included: unavailability of the Infantometer, the requirement for two operators to use the Infantometer, a lack of instructions on how to use the Infantometer and unfamiliarity with the Infantometer. The is summarised in Table 3.
Table 3. Reason behind preference of measurement practice.
| |
Why do you prefer this method |
| |
It is quicker (%) |
Easier to perform (%) |
Easily accessible (%) |
More accurate (%) |
Other reason (%) |
| Tape-measure |
21.2 |
27.3 |
33.3 |
6.1 |
12.1 |
| Infantometer |
6.5 |
19.4 |
12.9 |
61.3 |
0.0 |
(p<0.001)
Of all the survey participants, 92.6% (95%CI: 0.8457, 0.9723) responded YES to introduce and implement the Infantometer at the hospital to enhance the quality of care for newborns. However, those who responded NO to implementing the Infantometer were given the opportunity to voice their concerns. Concerns raised included practicality, storage issues, responsibility for maintenance, the actual benefit to women and newborns, potential discomfort for the newborn and the possibility of workforce deskilling in the use of the Tape-measure method if the Infantometer becomes the standard.
| | | | Discussion | The survey provides valuable insights into newborn length measurement practice at the hospital. The Tape-measure method is predominantly used with its speed and accessibility being cited as the main advantages. The survey data suggests significant differences in the use of the Infantometer between nurses and midwives, with 57.9% of nurses compared with 5.1% of midwives utilising the Infantometer.
There was also a significant variability in the tool used for newborn length measurement across the different wards. Survey respondents from the Labour ward, Special care nursery and Post-natal ward predominantly utilised the Tape-measure method, whilst those from the Paediatric ward exclusively utilised the Infantometer for newborn length measurement.
The survey data highlights the inconsistent use of the Infantometer at the hospital. It also indicates that providing Infantometer training to the Paediatric ward may yield limited benefit as the ward already exclusively uses the Infantometer. Focusing Infantometer training on midwives and staff in the Labour, Special Care Nursery and Post-natal wards could be more resource efficient.
Among users of the Tape-measure method, 65.7% of all were unaware of the Infantometer in the survey. This statistic was similar between both nurses and midwives. This suggests that differences in usage between nurses and midwives may not be attributed to differences in awareness of the Infantometer but instead could reflect variations in training, accessibility or ward-specific practices.
However, every single survey respondent who was not aware of the Infantometer responded YES to learning how to use it. Moreover, 91.0% (95%CI: 0.8152, 0.9664) of all survey respondents using the Tape-measure method, regardless of their awareness of the Infantometer, were open to adopting the Infantometer as a standard practice to enhance quality of care. This positive attitude indicates a high level of adaptability among the staff, and suggests that resistance from staff is unlikely to pose a significant obstacle in the transition to the Infantometer as standard practice.
Those who utilized the Infantometer preferred it for its accuracy and the Tape-measure method was preferred for its speed and accessibility on the ward. The preference between the two methods suggests that Tape-method users are willing to trade-off accuracy for speed in the measurement process. Therefore, an Infantometer training program should emphasize the importance of accurate newborn length measurement and explain why it justifies the trade-off in speed when compared to the Tape-measure method.
Furthermore, for an Infantometer training program at the hospital and sites alike, it must recognize the existing lack of awareness of the Infantometer, and therefore, it should not presume any prior knowledge about the Infantometer amongst the participants of the training program. It should offer comprehensive education on its usage to facilitate a seamless transition. This training could be delivered through face-to-face sessions and instructional videos, offering guidance to healthcare staff on the proper utilization of the Infantometer and its importance to the care of the newborn.
Of the survey respondents that use the Infantometer as the tool for newborn length measurement, majority rated themselves as being very confident in using it, with an IQR of 8-10, and of those that primarily use the Tape-measure method but aware of the Infantometer, they had an IQR of 5-8 in confidence in using the Infantometer. This suggests that the latter group would also benefit from training in Infantometer, in order to bring their confidence up to par with those who already primarily use the Infantometer.
Concerns raised during the survey for implementing the Infantometer at the hospital, such as its practicality, storage, maintenance responsibility and the potential deskilling in the Tape-measure method if Infantometer becomes the standard, should be addressed in the Infantometer implementation plan. Developing strategies to address these concerns and providing ongoing support can contribute to the successful integration of the Infantometer into routine practice.
While the survey conducted at the hospital garnered a substantial number of responses, providing valuable insights, there are limitations of this survey which include:
1. Sample Size and Composition: The survey was completed by midwives and nurses at the hospital with a total of 81 responses. The sample size might not be large enough to represent all healthcare professionals involved in newborn length measurement, and majority of respondents were midwives (62/81), which could have inadvertently skewed the results.
2. Survey Method: The survey was voluntary and conducted online and could have led to self-selection bias. Those who are more interested or have stronger opinions might be more likely to respond.
3. Training and Implementation: the results suggest a training program could be beneficial. However, the effectiveness of such a program is not evaluated in this study. | | | | Conclusion | The survey conducted at the hospital reveals valuable insights into newborn length measurement practices. The Tape-measure method is predominantly used due to its speed and accessibility. However, the Infantometer, preferred for its accuracy, is inconsistently used across the different wards at the hospital. It suggests that perhaps a targeted training program, particularly for midwives and staff in the Labour ward, Special Care Nursery and Post-natal ward areas at the hospital, could be a more resource-efficient approach than providing training to all the staff involved in newborn length measurement.
There is also a lack of awareness of the Infantometer amongst survey participants using the Tape-measure method. The survey data suggests that the reason behind the popularity of the Tape-measure method at the hospital is a gap in training or awareness of the Infantometer rather than a preference for the Tape-measure method.
The survey data shows that resistance from staff is unlikely to pose a significant obstacle to the successful implementation of an Infantometer training program. It would be important for such a program to emphasize the importance of accurate newborn length measurement and explain why it justifies the trade-off in speed when compared to the Tape-measure method.
The training program should also address the existing lack of awareness about the Infantometer by not presuming any prior knowledge amongst its participants and offer comprehensive education on its usage.
Issues surrounding the Infantometer such as its storage, maintenance responsibility and the potential deskilling in Tape-measure method should be addressed in an Infantometer implementation plan.
By developing strategies to address these concerns and providing ongoing support, the Infantometer can be successfully integrated into routine practice in hospitals such as the hospital, to enhance the quality of care for newborns.2,3 | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- World Health Organisation. Training Course on Child Growth Assessment [Internet]. www.who.int. WHO; 2008 [cited 2023 Jun 10]. Available from: https://www.who.int/tools/child-growth-standards
- Wilshin J, Geary M, Persaud M, Hindmarsh P. The reliability of newborn length measurement. British Journal of Midwifery. 1999 Apr: 7(4):236-9. Available from https://doi.org/10.12968/bjom.1999.7.4.8349 [CrossRef]
- Wood, A.J., Raynes-Greenow, C.H., Carberry, A.E. and Jeffery, H.E., Neonatal length measurement inaccuracies. Journal of Paediatrics and Child Health. 2013 Feb 22: 49: 199-203. Available from https://doi.org/10.1111/jpc.12119 [CrossRef] [PubMed]
DOI: https://doi.org/10.7199/ped.oncall.2026.9
|
| Cite this article as: | | Modi V, Karunanayake M. A survey on newborn length measurement practice at an Australian metropolitan hospital. Pediatr Oncall J. 2025 Mar 07. doi: 10.7199/ped.oncall.2026.9 |
|