Ana Rita de Matos Ramos1, Isabel Maria do Amaral Rodeia Rodrigues de Brito1, Marta Ferreira Almeida2, José Paulo Alves Pinheiro Calhau1.
1Department of Paediatrics, Hospital Garcia de Orta E.P.E., Almada, Portugal,
2Department of Paediatrics, spital Garcia de Orta E.P.E., Almada, Portugal.
ADDRESS FOR CORRESPONDENCE
Ana Rita de Matos Ramos, Avenida Torrado da Silva, 2805-267, Almada, Portugal
Email: rita23ramos@gmail.com | | Abstract | Pyomyositis is a bacterial infection of striated muscle. It is a rare and potentially fatal pathology that usually progresses to intramuscular abscess. Its diagnosis can be difficult due to the clinical similarity with more frequent disorders. Magnetic Resonance Imaging (MRI) is the gold standard for an early diagnosis.
Most authors recommend percutaneous or surgical drainage followed by antibiotics (ATB), if an abscess is found. There are few cases described in the literature treated with exclusive ATB.
We report the case of an adolescent male with pyomyositis, and an abscess of the right internal obturator muscle successfully treated with conservative treatment. We aim to highlight that uncomplicated pyomyositis abscess in children may be managed without the need of percutaneous or surgical drainage. | | | | Keywords | | Pyomyositis, soft tissue infection, abscess, magnetic resonance imaging | | | | Introduction | Pyomyositis is a rare bacterial infection of the skeletal muscle that is often accompanied by intramuscular abscess formation. It is predominantly a disease of tropical countries and commonly occurs in the first and second decades of life, with a slight predominance in males.1,2
The etiology remains unclear, although some predisposing factors such as trauma, intense physical exercise, immunodeficiency, malnutrition and intravenous drug use are described.1,3 Staphylococcus aureus is the most frequent causative agent.2,3,4,5 Pyomyositis predominantly affects the muscles of the pelvic region and lower limbs, however, any muscle can be involved. Infection of the internal or external obturator muscles is extremely rare.1,2 The diagnosis is usually late, given the insidious clinical and overlapping symptoms with other pathologies. MRI remains the gold standard in the diagnosis of this pathology.4,5 Treatment of pyomyositis abscess has traditionally been based on percutaneous or surgical drainage followed by a prolonged course of ATB.
We describe a case of pelvic pyomyositis abscess of the internal obturator, in a previously healthy young sportsman, in which a conservative approach was adopted. There was a complete recovery, with no evidence of complications or sequelae.
| | | | Case Report | A previously healthy 17-year-old adolescent male was admitted to the pediatric emergency room due to six days of fever (40ºC, with chills), persistent pain in the right inguinal region and right iliac fossa (RIF) and anorexia. There was no history of recent travel or trauma. However, there was history of hockey training one day prior to onset of symptoms.
On admission, he was unwell but hemodynamically stable; RIF and right inguinal region were tender on superficial and deep palpation, without signs of peritoneal irritation. Internal rotation of the right hip was limited, and he could not walk; there were abrasions on both knees. The remaining examination was unremarkable. Abdominal and right hip ultrasound, bilateral radiography of the hip, abdominal-pelvic computed tomography (CT) scan and bone scintigraphy were normal. Laboratory evaluation: 4.7x10^9/L (95% neutrophils), C-reactive protein (CRP) 23.9 mg/dL, erythrocyte sedimentation rate 88 mm, creatine kinase (CK) 73 IU/L, HIV serology negative.
He was started on empirical ATB (intravenous ceftriaxone 100 mg/kg/day). It was changed to intravenous flucloxacillin on day 5, after Staphylococcus aureus was isolated from blood cultures.
He was apyrexic from day 1 of ATB but intense pain complaints lasted for the first nine days of hospitalization. On day 7, he underwent a pelvic MRI that showed an abscess of the right internal obturator muscle (28x49 mm) and a hyperintensity in the homolateral pubic bone consistent with osteomyelitis (Figure 1).
There was a slow but sustained improvement allowing the patient to be discharged home on day 19. By then, he had only mild pain, and was able to walk. There was also a reduction of inflammatory parameters (CRP 1.9 mg/dL in Day 13 of hospitalization) and slight reduction of the dimensions of the internal obturator muscle abscess to 20x45 mm in MRI performed at Day 14.
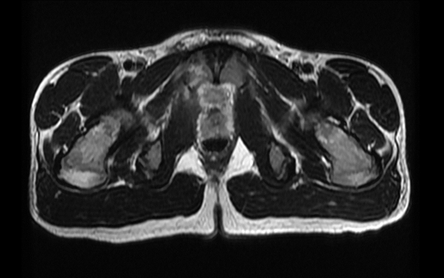
He was kept on oral flucloxacillin (1g tds) for a ten-week-total of ATB. There was consistent improvement during clinical and analytical follow-up. Two months after the first MRI, a new one showed abscess resolution and mild inflammatory signs of the internal obturator muscle and right pubis (Figure 2). Eight months after diagnosis, he was clinically well and had a normal MRI.
Figure 1. Arrow: Thickening and hyperintensity in the T2-weighted sequences of the right internal obturator muscle, where a 28x49mm lobulated collection is identified. Arrowhead: Hyperintensity of the right pubic body in the context of osteomyelitis.
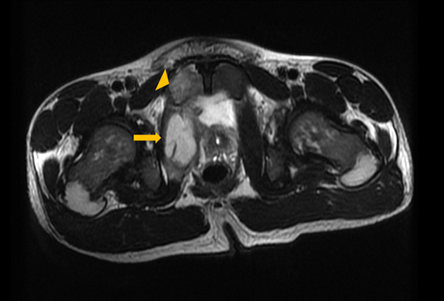
Figure 2. Resolution of the abscess formation. Persistence of mild inflammatory signs in the right internal obturator muscle and pubis.
 | | | | Discussion | Pyomyositis is a bacterial infection of the skeletal muscle, commonly associated with abscess formation. It was first described by Scriba in 1885 as an endemic disease of tropical areas, so is therefore known as tropical pyomyositis.3 Although less frequent in temperate climates, several studies have shown an increase in incidence in recent decades.1,2,3,6 In these regions, pyomyositis is often associated with immunodeficiency states (HIV infection), cancer, diabetes mellitus or intravenous drug use. However, it can occur in young and healthy individuals, especially after vigorous physical exercise or local trauma, as happened in our patient. Since the skeletal muscle is naturally resistant to infection, it is postulated that for pyomyositis to occur, it is necessary to comply with two premises: presence of damaged muscle area and transient bacteremia.7,8,9 In our case, the boy reported a hockey training on the day before the complaints and examination revealed abrasions in both knees which may have functioned as a facilitating factor for the infection.
The natural history of pyomyositis encompasses three phases that are evolutionary: the invasive phase lasts 10 to 21 days and it is characterized by insidious onset of pain and muscle edema accompanied by gait claudication; only 2% of patients are diagnosed at this stage. In the second phase (purulent/suppurative) complaints become more intense, the muscle involved becomes painful on palpation and local inflammatory signs may arise; fever and general malaise are frequent; intramuscular abscess formation commonly occurs at this stage. In the absence of diagnosis and targeted treatment, progression to the last stage of the disease occurs, marked by local and distant septic complications, with possible progression to septic shock and death.3,10,11,12,13
The diagnostic delay is due to nonspecificity of symptoms and clinical overlap with other more frequent pathologies like appendicitis or septic arthritis. The fact that our patient's pyomyositis involved the internal obturator muscle (an extremely rare location) made diagnosis even more difficult due to the deep location of this muscle not accessible for direct examination and whose manifestation with inflammatory signs of the skin is rare.
Laboratory findings in pyomyositis are nonspecific and transversal to other infectious pathologies. Leukocytosis and neutrophilia are present in 50-60% of cases and inflammatory markers (ESR and CRP) are universally increased.3,4 On the other hand, CK values are often normal because the abscess develops between muscle fibers, without myocyte damage.3 In pyomyositis, only 2/3 of patients have positive blood cultures.3 Staphylococcus aureus is the most commonly found pathogen (70-90% of the cases), however, Streptococcus pyogenes, Enterococcus and Escherichia coli are other possible agents.3
In this case, all initial imaging tests were considered normal, which contributed to the diagnostic challenge. Conventional radiography has little diagnostic value on pyomyositis except in the rare cases of bone involvement.3 Ultrasound is a widely available technique, but it can fail the diagnosis, especially in the early stages of the disease or in cases of deep muscle involvement.4 The high sensitivity (85%) of bone scintigraphy allows the detection of subtle and early functional changes without anatomical translation in radiological studies; however, it is a low-specificity test (25%), so it should not be a first-line exam.14,15 The CT scan can identify muscle abscesses, but it fails to identify early inflammatory changes.1,2,3,4 MRI is the gold standard for diagnosis of pyomyositis, presenting sensitivity of 97% and specificity of 92%5; it has a high spatial resolution and the use of contrast allows the distinction between inflammatory processes, abscesses, septic arthritis and osteomyelitis. In our case, the diagnosis was made based on MRI findings.
Pyomyositis can be a multifocal disease in 15 to 43% of cases3, which didn’t occur in our patient. The identification of the focus of osteomyelitis in the homolateral pubic bone was considered a local complication, by direct extension of the infectious process.
Early diagnosis and institution of therapy seems to be the main factors for the final prognosis of the disease. While in stage I ATB seems to be sufficient, in complicated abscess pyomyositis most authors recommend percutaneous or surgical drainage followed by a prolonged course of ATB. The most appropriate duration of therapy has not yet been established, but most authors use a regimen of intravenous followed by oral therapy for a total of 3-8 weeks.2 To date, there are few cases described in the literature successfully treated through conservative treatment.2,3 In our case, the favorable progress made us not drain the abscess. However, we opted to maintain a longer course of ATB, until complete resolution of symptoms and imaging findings.
In this case, the precocious initiation of ATB, even before the diagnosis was established, may have been a decisive factor in the good clinical progress of the patient. Therefore, while facing a case of pyomyositis with abscess, we recommend the early institution of antibiotics as monotherapy, followed by close monitoring of clinical, biochemical and imaging evolution. Surgical or percutaneous drainage is an invasive, not risk-free procedure, but should be accomplished in case of deterioration and disease progression. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Comegna L, Guidone P, Prezioso G, Franchini, S, Petrosino M, Filippo P, et al. Pyomyositis is not only a tropical pathology: a case series. J Med Case Rep 2016; 10:372-377. [CrossRef] [PubMed] [PMC free article]
- Miller N, Duncan R, Huntley J. The conservative management of primary pyomyositis abscess in children: case series and review of the literature. Scott Med J 2011; 56:i-181. [CrossRef] [PubMed]
- Mitsionis G, Manoudis G, Lykissas M, Sionti J, Motsis E, Georgoulis A, et al. Pyomyositis in children: early diagnosis and treatment. J Pediatr Surg 2009;44:2173-8. [CrossRef] [PubMed]
- Moressa V, Pastore S, Naviglio S, Ventura A. A young goalkeeper with buttock pain and fever. BMJ 2017;357: j2400. [CrossRef] [PubMed]
- Bodman C, Ceroni D, Dufour J, Crisinel P, Bourgeois A, Zambelli P. Obturator externus abscess in a 9-year-old child. A case report and literature review. Medicine 2017; 96:e6203. [CrossRef] [PubMed] [PMC free article]
- White S, Stopka S, Nimityongskul P, Jorgensen D. Transgluteal Approach for Drainage of Obturator Internus Abscess in Pediatric Patients. J Pediatr Orthop. 2017;37: e62-e66. [CrossRef] [PubMed]
- Park E, Chilstrom M. Diagnosis of Pyomyositis in a Pediatric Patient with Point-of-Care Ultrasound. Western Journal of Emergency Medicine. 2016; 4: 464-465. [CrossRef] [PubMed] [PMC free article]
- Waseem M, Kumari D, Toledano T. Fever and Hip Pain. Not Always Due to a Septic Hip. Pediatric Emergency Care. 2018; 34: e236-e238. [CrossRef] [PubMed]
- Fowler T, Strote J. Isolated obturator externus muscle abscess presenting as hip pain.2006; 30: 137-139. [CrossRef] [PubMed]
- Gubbay AJ, Isaacs D. Pyomyositis in children. Pediatr Infect Dis J. 2000; 19:1009-12. [CrossRef] [PubMed]
- Kiran M, Mohamed S, Newton A, George H, Garg N, Bruce C. Pelvic pyomyositis in children: changing trends in occurrence and management. Int Orthop. 2018;42: 1143-1147. [CrossRef] [PubMed]
- Klein-Kremer A, Jassar H, Nachtigal A, Zeina A. Primary pyomyositis in a young boy: clinical and radiologic features. Isr Med Assoc J. 2010;12: 511-3.
- Prasad R, Verma N, Mishra OP. Pyomositis: a report of three cases. Ann Trop Paediatr. 2009; 29: 313-6. [CrossRef] [PubMed]
- Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009;23:80-9. [CrossRef] [PubMed] [PMC free article]
- Lemonick DM. Non-tropical pyomyositis caused by methicillin-resistant Staphylococcus aureus: an unusual cause of bilateral leg pain. J Emerg Med. 2012;42:e55-62. [CrossRef] [PubMed]
DOI: https://doi.org/10.7199/ped.oncall.2022.29
|
| Cite this article as: | | Ramos A R d M, Brito I M d A R R d, Almeida M F, Calhau J P A P. Pelvic pyomyositis and abscess of the internal obturator muscle: case successfully managed with conservative treatment. Pediatr Oncall J. 2022;19: 89-91. doi: 10.7199/ped.oncall.2022.29 |
|