Catarina Andrade1, Beatriz Câmara1, Sónia Freitas2, Cristina Freitas1, Paulo Sousa1.
1Pediatrics, Hospital Central do Funchal, SESARAM, EPERAM, Funchal, Portugal,
2Dr. Maria Isabel Mendonça Research Center, SESARAM, EPERAM, Funchal, Portugal.
ADDRESS FOR CORRESPONDENCE
Catarina Andrade, Avenida Luís de Camões, n.º 57; 9004-514 Funchal
Email: catajandrade@gmail.com | | Abstract | Introduction: Sleep is crucial for physiological balance. Despite being neurobiologically determined, it is influenced by behavior. Sleep disturbances affect 20-30% of children and adolescents, with biopsychosocial consequences and risk of persistence into adulthood. This study aims to explore sleep patterns among children, assess the prevalence and impacts of sleep disturbances, and determine associated risk factors to support the establishment of a sleep consultation service.
Methods: Epidemiological, observational, cross-sectional study of sleep habits in children aged 6-10 years in an island region. The Portuguese version of the Children Sleep Habits Questionnaire and questions for epidemiological characterization were administered to caregivers from February to June 2022. Statistical analysis was conducted using SPSS version 25.0.
Results: The study garnered 507 responses, with no sex predominance and a median age of 8 years. Around 36.3% exhibited signs of sleep disturbances, unrelated to age or sex. Discrepancies were noted between caregivers' perceptions and actual disturbances. Variations in sleep schedules between weekdays and weekends were observed, along with a link between sleep issues and health problems like allergies, school performance, sports activities, and caffeine intake, but not with screen time, even though 26% exceeded two hours of daily screen use. The mean BMI in the sleep disturbance group was higher, but not statistically significant. A positive correlation was evident between the total sleep duration of children and their caregivers.
Conclusions: The observed high prevalence of sleep disturbances aligns with existing literature and highlights the necessity for healthcare interventions and enhanced education on sleep hygiene.
| | | | Keywords | Sleep Habits; Sleep Quality; Sleep Deprivation; Primary Schools; Caregivers.
Abbreviations: CSHQ-PT - Children Sleep Habits Questionnaire; IgE - Immunoglobulin E; NREM - Non-Rapid Eye Movement; OSAS - Obstructive Sleep Apnea Syndrome; REM - Rapid Eye Movement; SD - Standard Deviation; SPP - Portuguese Society of Pediatrics. | | | | Introduction | Sleep is defined as a restorative physiological state, characterized by the suppression of cortical functions, reduced perception and response to stimuli, and a decrease in muscle tone, heart rate, and respiratory rate. Sleep is crucial for maintaining physiological balance among various systems, contributing to energy conservation, thermoregulation, cardiovascular functions, immune responses, and endocrine-metabolic activities, such as growth hormone production and appetite regulation. It also plays a significant role in cognitive functions, including memory consolidation and mood regulation.1
Humans spend about one-third of their life sleeping. The alternation between wakefulness and sleep constitutes a fundamental rhythm, dependent on homeostatic and circadian processes, and is particularly significant during childhood. Throughout development, there is a progressive maturation in the organization of sleep, characterized by a reduction in total daily sleep time and a convergence towards adult patterns, with alternating periods of REM (Rapid Eye Movement) and NREM (Non-Rapid Eye Movement) sleep in increasingly prolonged cycles, and a decrease in the REM/NREM ratio.2,3 In this context, consensuses have been established for normative sleep patterns in pediatric ages. The Portuguese Society of Pediatrics (SPP) offers specific recommendations for sleep duration and nap times according to age, similar to the American Academy of Pediatrics, which has previously emphasized the importance of establishing sleep duration guidelines as a health-promoting measure.4,5
Sleep may be deemed inadequate due to alterations in duration or quality. Although it is a neurobiologically determined process, it is significantly influenced by behavioral components. Consequently, among many factors, sleep habits are modulated by the interaction with and examples set by caregivers, beliefs, established routines and rules, and the sleeping environment.6 Thus, it is essential to establish sleep hygiene measures from the first year of life, reinforcing them throughout development, especially during stages of increased independence, such as school age. Comorbidities that impact sleep quality, such as developmental, neurological and/or respiratory disorders, and obesity, are also recognized.7
Sleep disturbances, affecting 20-30% of children and adolescents, are categorically classified according to the International Classification of Sleep Disorders into: sleep-related breathing disorders, sleep-related movement disorders, parasomnias, insomnia, central disorders of hypersomnolence, circadian rhythm disorders, and other sleep disturbances.8,9 Sleep deprivation can lead to daytime consequences which may also serve as warning signs for diagnosing these nosological entities, including excessive sleepiness, irritability, behavioral/mood changes, compromised academic performance, increased risk of accidents, hypertension, and obesity. Concurrently, these issues contribute to increased susceptibility to family dysfunction by also affecting the duration and quality of the parents’ sleep.7 The lack of identification and management of sleep problems can contribute to their persistence into adulthood, making timely diagnosis and intervention crucial.
The current study aims to characterize sleep habits in order to assess the prevalence of sleep disturbances in the general school-aged population, identify associated risk factors and consequences, and evaluate the relevance of establishing a Sleep Consultation Service within a Pediatric Department of a Tertiary Hospital. | | | | Methods & Materials | Study Design
An epidemiological, observational, and cross-sectional study was conducted to characterize the sleep habits of school-aged children in the Madeira Islands, utilizing a questionnaire administered to caregivers.
Target Population and Sample
The study targeted all children aged 6 to 10 years residing in the Madeira Islands. Based on a total of 10457 children in this age group living in the region in 2020, according to estimates from the Regional Directorate of Statistics of Madeira, a sample size of at least 313 participants was calculated for a 95% confidence level and a 5% margin of error, using the OpenEpi statistical tool.
The sample was formed based on the willingness of caregivers to complete the questionnaire. In this context, inclusion criteria were set as follows: children aged between 6 and 10 years, completion of the entire questionnaire, and affirmative compliance with informed consent.
Data Collection
Data were collected through the administration of a questionnaire to caregivers at all public and private primary education institutions between February and June 2022. The questionnaire was distributed digitally via Google Forms, in collaboration with the Regional Secretary of Health and Civil Protection, the Regional Secretary of Education, Science and Technology, and the educational institutions in the Madeira Islands, to ensure data protection.
Legal guardians of the participants provided informed consent for the collection, analysis, and publication of the data. The study was approved by the Ethics Committee of SESARAM, EPERAM (S.22001836/2022).
Instruments
The questionnaire included a first part (Supplemental material), which is the Portuguese version of the Children Sleep Habits Questionnaire (CSHQ-PT). It aims to assess caregivers' perception of the existence of sleep problems, characterize sleep habits, and identify potential sleep disturbances through questions related to the main signs and symptoms. It consists of 45 questions divided into the following domains: "bedtime", "behavior during sleep", "waking in the morning", and "daytime sleepiness". Responses are based on the previous week's reference period and are categorized as "rarely" (once a week or never), "sometimes" (two to four times a week), and "usually" (five to seven times a week). Responses are scored from one to three points, respectively (except for items marked in the questionnaire which are scored inversely), with a higher total score suggesting more sleep problems. The original questionnaire's authors defined the Sleep Disturbance Index by summing 33 of the 45 items, which were conceptually organized into eight subscales related to sleep problems, namely: "bedtime resistance", "sleep onset", "sleep duration", "sleep anxiety", "night awakenings", "parasomnias", "sleep breathing disorders", and "daytime sleepiness”.7,10 The Children Sleep Habits Questionnaire has been validated for the Portuguese population aged 2 to 10 years, with a cut-off point of 48 points established for screening sleep disturbance, with a sensitivity of 83% and specificity of 69%.7,11
The second part of the questionnaire (Supplemental material) served as a complement for epidemiological characterization, including analyses of somatometry, pathological history, academic performance, physical exercise, screen exposure, dietary patterns, and social context, including the sleep habits of caregivers.
Data Analysis
For binary variables, clinical characteristics were presented as frequencies. Data for continuous variables were reported as mean ± standard deviation (SD); for non-normal distributions, median (minimum-maximum) was shown. The Chi-square test was applied to categorical variables and the Student's t-test or Mann-Whitney test was used for numerical variables, as appropriate. Spearman’s correlation was utilized to analyze relationships between variables. Statistical analysis was conducted using SPSS version 25.0 (IBM, Armonk, NY, USA). All p-values were two-tailed and considered statistically significant at p<0.05.
| | | | Results | A total of 536 responses to the questionnaire were obtained, with 29 participants excluded: 18 due to lack of consent, 9 for not meeting the age-related inclusion criteria, and 2 due to duplicate entries. This resulted in a final sample of 507 children, which is representative of the target population. The questionnaires were predominantly completed by mothers (466; 91.9%), with the remaining 41 filled out by fathers (36; 7.1%) and other household members (5; 1.0%).
Regarding the sample characterization, 253 (49.9%) participants were female and 254 (50.1%) were male, with a median age of 8.0 years (Table 1). The average sleep duration was slightly higher in females (9.41 hours vs. 9.32 hours), though not statistically significant (p=0.277). A negative correlation was established between total sleep duration and child's age, but this was not statistically significant (p=0.438).
Table 1. Sociodemographic characterization of the children and their responsible caregivers in the sample.
| Variable |
n |
% |
Variable |
n |
% |
| Child's gender |
Age of female/male caregivers |
| Female |
253 |
49,9 |
<20 years |
1/0 |
0,2/0,0 |
| 20-30 years |
40/14 |
7,9/2,8 |
| 30-40 years |
228/176 |
45,0/34,7 |
| Male |
254 |
50,1 |
40-50 years |
231/280 |
45,6/55,2 |
| >50 years |
7/37 |
1,4/7,3 |
| Child's age |
Educational qualifications of female/male caregivers |
| 6 years |
110 |
21,7 |
4th grade |
10/33 |
2,0/6,5 |
| 7 years |
126 |
24,9 |
6th grade |
31/81 |
6,1/16,0 |
| 8 years |
93 |
18,3 |
9th grade |
82/128 |
16,2/25,2 |
| 9 years |
118 |
3,3 |
12th grade |
180/138 |
35,5/27,2 |
| 10 years |
60 |
11,8 |
Bachelor's degree |
172/96 |
33,9/18,9 |
| |
|
|
Master's degree |
30/27 |
5,9/5,3 |
| |
|
|
Doctorate |
2/4 |
0,4/0,8 |
In the total score of the CSHQ-PT, a median of 45.0 points (range 33-76; maximum possible 99 points) was observed, with no relationship to sex (p=0.827) or age (p=0.115) (Figure 1). A strong and positive correlation was found between the subscale scores (Table 2) and the total questionnaire score, except for subscale 2, labeled "sleep onset," where the only item is scored inversely ("Usually" = 1; "Sometimes" = 2; "Rarely" = 3). Among the participants, 184 (36.3%) scored above 48 points, indicative of a screening compatible with sleep disturbance. In contrast, only 77 (15.2%) of the caregivers affirmatively answered the initial question regarding whether they considered the child to have any sleep or falling asleep problems. Consequently, a significant difference (p<0.0001) was established between the caregivers’ perception and the presence of disturbance as objectively measured by the questionnaire.
Figure 1. Distribution of total CSHQ-PT scores by age.
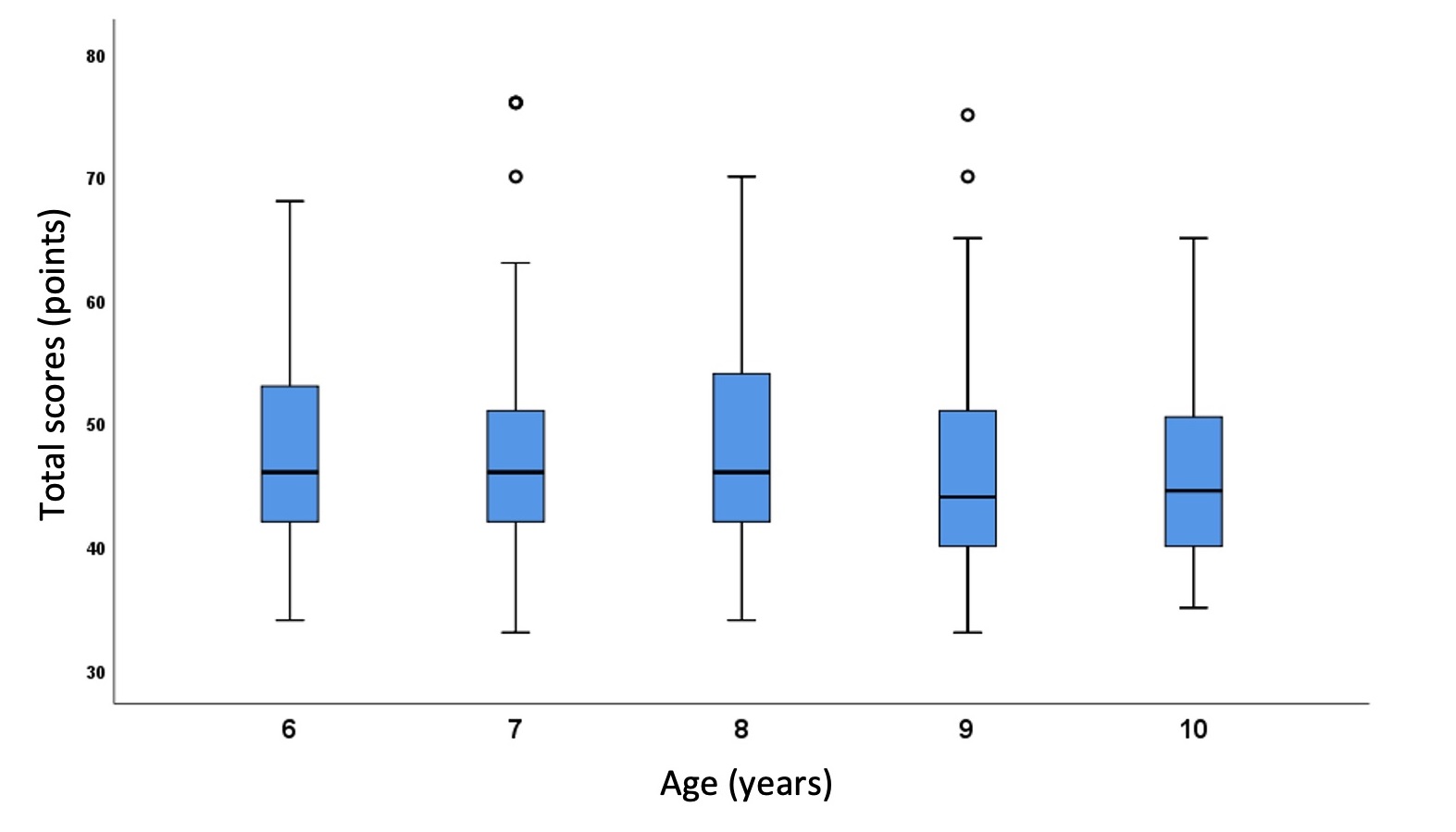
Table 2. Scores by subscales of the CSHQ-PT.
Subscales
(Min-Max) |
Median Score |
"Bedtime resistance”
(6-18) |
8 |
"Sleep onset"
(1-3) |
2 |
“Sleep duration”
(3-9) |
3 |
“Sleep anxiety”
(4-12) |
6 |
"Night awakenings”
(3-9) |
3 |
“Parasomnias”
(7-19) |
8 |
“Sleep breathing disorders”
(3-9) |
3 |
“Daytime sleepiness”
(8-23) |
13 |
Among the risk factors related to daily sleep routines, it is noteworthy that bedtime responses on weekdays ranged from 19:30 to 23:30 and on weekends from 21:00 to 23:50. Meanwhile, the range of wake-up times on weekdays was between 06:00 and 10:00 and on weekends between 06:30 and 12:00. A significant variation was demonstrated between weekday and weekend sleep schedules (p<0.0001). It is important to note regarding the regularity and consistency of sleep habits, in the item "Goes to bed at the same time every day," only 7 (1.4%) participants indicated "Usually," and in the item "Sleeps the same number of hours every day," only 20 (3.9%) participants recorded "Usually." The average total sleep duration was significantly higher in the group of children without sleep disturbances (p<0.0001). Regarding autonomy at bedtime, it is important to mention the item "Falls asleep alone in their own bed," where 307 (60.6%) participants indicated "Rarely".
The results demonstrated that children who engage in sports activities exhibit less sleep disturbance compared to those who do not (p=0.037), regardless of the duration of the exercise (p=0.296) and the time interval between exercise and bedtime (p=0.156). No significant differences were found between the time interval from the last meal to bedtime and the presence of sleep disturbances (p=0.061). However, significant differences were observed between the consumption of caffeinated beverages and the presence of sleep disturbances (p=0.017). Regarding screen exposure, no statistically significant results were established between the total daily usage duration (p=0.220), use in the bedroom (p=0.210), and the time interval between use and bedtime (p=0.204) and the presence of disturbances, although it is noteworthy that 26.2% (133) of the sample used screens for more than two hours per day.
Regarding risk factors associated with personal medical history, 42.0% (213) reported health issues, particularly allergic conditions - "rhinitis" 122 (24.1%), "asthma" 53 (10.5%), and "atopic skin" 82 (16.2%). Additionally, 25% (127) of the sample reported having multiple medical conditions. Among neurodevelopmental disorders, 31 (6.1%) indicated "speech difficulties," 45 (8.9%) "learning difficulties," 43 (8.5%) "hyperactivity or attention problems," and 9 (1.8%) "autism". It was demonstrated that children with pathological antecedents have a significantly increased risk for the presence of sleep disturbances (p<0.0001), unrelated to regular medication intake (p=0.287), despite 82 (16.2%) participants being reported to take usual medications, mostly non-sedative antihistamines. The average Body Mass Index was higher in the group with sleep disturbances, but not statistically significant (p=0.468). Among participants, 7 (1.4%) exhibited possible nocturnal enuresis, marking "Sometimes" or "Usually" for the item "Wets the bed at night".
For the "Sleep-Related Breathing Disorders" subscale, an average score of 3.6 points was observed. Among the responses, 36 (7.1%) participants indicated "Sometimes" or "Usually" for "Snores loudly," 15 (3.0%) for "Appears to stop breathing during sleep," and 22 (4.3%) for "Snores or has difficulty breathing".
Regarding social context risk factors, total sleep duration showed a negative correlation with the age of both female and male caregivers (Table 1), although not statistically significant (p=0.263 and p=0.591, respectively). It also demonstrated a positive correlation with the educational qualifications of both female and male caregivers (Table 1), again without statistical significance (p=0.567 and p=0.170, respectively). A significant positive correlation was evident between the total sleep duration of the child and that of the female caregiver (r=0.133, p=0.003) and the male caregiver (r=0.148, p=0.001). No significant differences were found regarding sleep disturbances in children between single-parent and nuclear family households (p=0.885).
To assess the consequences of sleep disruption, the impact on academic performance was evaluated. No significant differences were found regarding sleep disturbances across the four years of primary education (p=0.402). In the subjects of Portuguese Language and Mathematics, statistically significant differences were observed between the final grades (Table 3) and the presence of sleep disturbances (p=0.005 and p=0.009, respectively). No such correlation was established for the subject of Environmental Studies (p=0.285).
Table 3. Academic performance in the previous period of the children studied.
| Disciplina |
Grade |
| Very Good |
Good |
Satisfactory |
Unsatisfactory |
| n |
% |
n |
% |
n |
% |
n |
% |
| Portuguese Language |
226 |
44,6 |
189 |
37,3 |
86 |
17 |
6 |
1,2 |
| Mathematics |
228 |
45 |
199 |
39,3 |
71 |
14 |
9 |
1,8 |
| Environmental Studies |
301 |
59,4 |
151 |
29,8 |
49 |
9,7 |
6 |
1,2 |
| | | | Discussion | Sleep in pediatric ages has garnered increasing attention from the scientific community, due to the recognition of its importance for overall health, as well as the consequences that disturbances entail.
Until this study, the characterization of sleep habits among children in the Madeira Islands had not been documented. For this reason, the study targeted the school-aged community to avoid biases inherent in more circumscribed subgroups, using a previously validated questionnaire. Although it is a subjective instrument, it allows for the collection of a larger number of responses in a population-based screening, with the questionnaire being completed by responsible adults in the participants' natural environment, without associated costs.7
The average sleep duration of the sample under study falls within the 9 to 11 hours recommended by the Portuguese Society of Pediatrics (SPP) for the age group of 6 to 10 years, without significant differences between genders and with a tendency for shorter duration as age increases, which is expected in the progression towards the adult sleep pattern.2 Mendes et al. (2004), in a study characterizing the sleep habits of school-aged children residing in Lisbon, recorded an average nighttime sleep duration also within the appropriate range (9.8 hours), similar to that described for other regions of the country.12 The study by Silva (2014), which also used the CSHQ-PT, targeted children aged 2 to 10 years residing in Lisbon, Setúbal, and Alentejo, documented an average nighttime sleep duration that decreased from 10.1 hours at age 6 to 9.7 hours at age 10, also showing no differences between genders.7 Indeed, there is no evidence in the literature supporting the effect of gender on sleep patterns in school-aged children, hence the recommendations are similar for both genders.13
In the current study, 36.3% of participants scored above the threshold consistent with sleep disturbances, a value higher than the prevalence of sleep disturbances reported in the literature, but consistent with Silva's 2014 study, which revealed a positive screening in 39% of children.7,8 Interestingly, our study found a significant discrepancy between the number of participants with scores suggestive of sleep disturbance and the perception of the caregivers, a phenomenon also noted in Silva's 2004 study, where the prevalence of sleep problems from the parents' perspective was only 10.4%, roughly a quarter of the percentage of participants with disturbances according to the questionnaire.7 The lack of recognition of the prevalence of sleep problems by caregivers may suggest a relative tolerance for behavioral issues associated with sleep, as well as unawareness of children's actual sleep needs, underscoring the urgency for investment in health literacy that emphasizes the importance of sleep.
Similar to findings by Silva (2014), our study also observed a later bedtime and wake-up time on weekends, with significant variation compared to weekdays, as well as a lack of consistency in sleep routines.7 In school-age children, greater autonomy in the sleep onset process is expected, a finding not demonstrated in the present study. This contrasts with the studies by Silva (2014) and Clemente (1997), where the percentages of children who usually fell asleep alone in their beds were significantly higher, at 72% and 73.8% respectively.7,14 The findings of our study support what is reported in the literature regarding the presence of a cultural influence, where countries in Southern Europe are characterized by later and more irregular sleep schedules and greater parental involvement at bedtime.15 These results enable us to identify various risk factors inherent to poor sleep hygiene and crucial to the percentage of sleep disturbances reported, despite the average total sleep duration being adequate.
Physical activity was associated with less sleep disturbance, which is supported by literature suggesting that exercise impacts sleep efficiency, continuity, and architecture, and is proposed as a non-pharmacological measure for managing sleep disturbances.16 Although our study did not demonstrate a significant relationship between screen exposure and the presence of sleep disturbances, literature has shown that screen time is associated with delays in bedtime and consequently impacts the total duration of sleep.17 Additionally, multifactorial approaches show that high levels of physical activity (≥60 minutes of moderate to vigorous activity per day), low levels of sedentary behavior (≤2 hours of screen exposure per day), and adequate sleep duration (9 to 11 hours per night) are synergistic in their beneficial impact on mental health indicators in children and adolescents.18
Caffeine intake was associated with the presence of sleep disturbances, noteworthy is that caffeine can be found in children's diets through elements other than coffee itself, notably in energy drinks increasingly consumed among the young population. Although data in the literature are limited, the impact of caffeine appears to be related not just to the dose but also to the time interval between ingestion and bedtime, with shorter intervals leading to increased sleep latency, similar to what is described in adults.19
Regarding pathological antecedents, there was a predominance of pathologies related to atopy. Indeed, in a retrospective study by Zhang (2016) on children undergoing treatment for snoring, a significantly higher proportion of abnormal total serum Immunoglobulin E (IgE) levels was demonstrated in children with severe Obstructive Sleep Apnea Syndrome (OSAS) compared to those with mild to moderate OSAS. The authors concluded that allergic sensitization could contribute to the exacerbation of an underlying OSAS.20 Particularly in the case of rhinitis, symptoms that interfere with sleep are common, and it is documented that therapies reducing nasal congestion can impact sleep quality. Therefore, identifying and treating rhinitis are important steps to prevent the deterioration of sleep quality in children with underlying sleep-related breathing disorders.21
Regarding the subscale titled “Sleep-Related Breathing Disorders”, the current study achieved an average score that is comparable to the average obtained in Silva's 2014 study.7 According to parental perception, breathing pauses were noted in 3.0% of participants, a figure that aligns with the prevalence of 1.2%–5.7% described in the literature for OSAS. This finding should be appropriately assessed with objective and standardized sleep studies.22
According to the literature, sleep disturbances are particularly common in children with neurodevelopmental disorders. This association may be caused by neurobiological mechanisms underlying the pathophysiology and/or by symptoms inherent to the neurodevelopmental disorder itself.7 The estimated incidence of sleep disturbances ranges from 32-71.5% in children with autism spectrum disorders, 25-50% in children with attention deficit hyperactivity disorder, and 24-86% in children with unspecified intellectual deficits. Besides being common, sleep disturbances in these groups tend to be chronic. Early recognition and management of these disturbances have an impact on functional abilities, treatment response, and quality of life for these patients and their families.23 However, it is necessary to consider that certain behavioral changes, such as irritability and restlessness, which do not fully meet the criteria for a neurodevelopmental disorder, can be signs of sleep deprivation, without the obvious presence of excessive daytime sleepiness.24
In our sample, a higher average Body Mass Index was documented in children with sleep disturbances, which corroborates data from the literature supporting a cross-sectional and longitudinal association between sleep duration and obesity.25 This is a multifactorial association, influenced by variables such as diet. Moreira et al. (2010), in a study on dietary patterns among 1976 Portuguese children aged 5 to 10 years, found that longer sleep duration was positively associated with a healthier diet.26 Data extrapolated from adults reiterate hormonal mechanisms to explain the association between sleep duration and obesity, with lower levels of leptin observed in individuals experiencing sleep deprivation, consequently enhancing signals for caloric intake.27
Regarding nocturnal enuresis, its association with sleep-related breathing disorders is well documented in the literature. However, it is important to note that enuresis is significantly influenced by poor sleep hygiene.28
Concerning risk factors related to the social context, a positive correlation was observed between the literacy level of responsible adults and the sleep duration of the child, similar to findings by Crispim et al. (2011). Less educated families constitute risk groups for sleep deprivation.29 A significant positive correlation was established between the total sleep duration of the child and the total sleep duration of the caregivers. This underscores that children's habits are shaped by the family's habits and that children's sleep disturbances have repercussions on the sleep of the rest of the family. Sleep deprivation in parents leads to daytime fatigue and mood changes, impacting parental performance.30
The literature emphasizes that sleep disturbances impair attention levels, learning capacity, memory, stimulus processing, and executive functions. Therefore, the impact on academic performance is an accurate measure to evaluate the consequences of sleep compromise in school-aged children, a finding that was evident in our study.31
The use of a validated questionnaire in a representative sample of school-aged children in the Madeira Islands will enable comparison with subsequent studies, as well as long-term monitoring of sleep habits.
However, it should be noted as a limitation that, like our study, most research characterizing sleep in pediatric ages is observational in nature, which allows for the identification of possible associations between variables but does not enable the establishment of cause-and-effect relationships. Additionally, the results were obtained through subjective and retrospective evaluation using a questionnaire, and are dependent on the perception of the caregivers. | | | | Conclusion | | In conclusion, the high prevalence of sleep disturbances identified corroborates literature data and justifies assessment by healthcare professionals. There is an urgent need for greater investment in education and motivation of populations regarding sleep hygiene, strategically beginning with education and health professionals. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Oliveira G, Saraiva J, eds. Lições de Pediatria. Vol I. Coimbra: Imprensa da Universidade de Coimbra; 2017. [CrossRef]
- Sociedade Portuguesa de Pediatria (SPP) - Secção de Pediatria Social (SPS). Recomendações SPS-SPP: Prática da Sesta da criança nas creches e infantários, públicos ou privados. Criança e Família. https://criancaefamilia.spp.pt/media/fwkj5qte/versao-educadores-e-pais_recomendacoes-sps-spp-sesta-na-crianca.pdf. June 1, 2017. Accessed July 10, 2024
- Galland B, Taylor B, Elder D, et al. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 2012; 16(3): 213-22. doi: 10.1016/j.smrv.2011.06.001. [CrossRef] [PubMed]
- Sociedade Portuguesa de Pediatria (SPP) e Associação Portuguesa do Sono (APS). Higiene do sono da criança e adolescente. Apsono. https://apsono.com/images/higienesono.pdf. Accessed July 10, 2024.
- Paruthi S, Brooks LJ, D'Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016; 12(6):785-786. doi: 10.5664/jcsm.5866. [CrossRef] [PubMed] [PMC free article]
- Mindell JA, Owens J. The Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Silva FMG. Hábitos e problemas do sono das crianças dos 2 aos 10 anos. In: Repositório da Universidade Nova de Lisboa [database online]. Faculdade de Ciências Médicas da Universidade Nova de Lisboa. https://run.unl.pt/handle/10362/14234. 2014. Accessed January 4, 2022.
- Bruni O, Novelli L. Sleep disorders in children. BMJ Clin Evid. 2010; 2010:2304.
- Darien Il, International classification of sleep disorders. 3rd ed. American Academy of Sleep Medicine; 2014.
- Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043-51. [CrossRef] [PubMed]
- Parreira AF, Martins A, Ribeiro F, et al. Clinical Validation of The Portuguese Version of the Children's Sleep Habits Questionnaire (CSHQ-PT) in Children with Sleep Disorder and ADHD. Acta Med Port. 2019;32(3):195-201. doi: 10.20344/amp.10906. [CrossRef] [PubMed]
- Mendes LR, Fernandes A, Garcia FT. Hábitos e perturbações do sono em crianças em idade escolar. Acta Pediatr Port. 2004; 35(4):341-347.
- Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003; 111(2):302-7. [CrossRef] [PubMed]
- Clemente V. Sono e Vigília em Crianças de Idade Escolar: Hábitos, comportamentos e problemas. Faculdade de Psicologia e Ciências da Educação, Universidade de Coimbra. 1997. Accessed July 15, 2024.
- Jenni OG, O'Connor BB. Children's Sleep: An Interplay Between Culture and Biology. Pediatrics. 2005; 115(1 Suppl):204-16. doi: 10.1542/peds.2004-0815B. [CrossRef] [PubMed]
- Dworak M, Wiater A, Alfer D, et al. Increased slow wave sleep and reduced stage 2 sleep in children depending on exercise intensity. Sleep Med. 2008; 9(3):266-72. doi: 10.1016/j.sleep.2007.04.017. [CrossRef] [PubMed]
- Hale L, Guan S. Screen Time and Sleep among School-Aged Children and Adolescents: A Systematic Literature Review. Sleep Med Rev. 2015; 21:50-8. doi: 10.1016/j.smrv.2014.07.007. [CrossRef] [PubMed] [PMC free article]
- Sampasa-Kanyinga H, Colman I, Goldfield GS, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2020;17(1):72. doi: 10.1186/s12966-020-00976-x. [CrossRef] [PubMed] [PMC free article]
- Wikoff D, Welsh BT, Henderson R, et al. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food and Chemical Toxicology. 2017; 109:585-648. doi: 10.1016/j.fct.2017.04.002. [CrossRef] [PubMed]
- Zhang J, Zhao J, Chen M, et al. Airway resistance and allergic sensitization in children with obstructive sleep apnea hypopnea syndrome. Pediatr Pulmonol. 2016; 51:426-30. doi: 10.1002/ppul.23264. [CrossRef] [PubMed]
- D'Elia C, Gozal Dm, Bruni O, et al. Allergic rhinitis and sleep disorders in children coexistence and reciprocal interactions. Pediatr (Rio J). 2022;98(5):444-454. doi: 10.1016/j.jped.2021.11.010. [CrossRef] [PubMed] [PMC free article]
- Ishman SL, Maturo S, Schwartz S, et al. Expert Consensus Statement: Management of Pediatric Persistent Obstructive Sleep Apnea After Adenotonsillectomy. Otolaryngol Head Neck Surg. 2023; 168(2): 115-130. doi:10.1002/ohn.159. [CrossRef] [PubMed] [PMC free article]
- Lihabi AA. A literature review of sleep problems and neurodevelopment disorders. Front Psychiatry. 2023; 14:1122344. doi: 10.3389/fpsyt.2023.1122344. [CrossRef] [PubMed] [PMC free article]
- Carter KA, Hathaway NE, Lettieri C. Common sleep disorders in children. Am Fam Physician. 2014;89(5):368-77.
- Matricciani L, Paquet C, Galland B, et al. Children's sleep and health: a meta-review. Sleep Med Rev. 2019; 46:136-150. doi: 10.1016/j.smrv.2019.04.011. [CrossRef] [PubMed]
- Moreira P, Santos S, Padrão P, et al. Food Patterns According to Sociodemographics, Physical Activity, Sleeping and Obesity in Portuguese Children. Int J Environ Res Public Health. 2010; 7(3): 1121-1138. doi: 10.3390/ijerph7031121. [CrossRef] [PubMed] [PMC free article]
- Leproult R, Cauter EV. Role of Sleep and Sleep Loss in Hormonal Release and Metabolism. Endocr Dev. 2010; 17:11-21. doi:10.1159/000262524. [CrossRef] [PubMed] [PMC free article]
- Choudhary B, Patil R, Bhatt GC, et al. Association of Sleep Disordered Breathing with Mono-Symptomatic Nocturnal Enuresis: A Study among School Children of Central India. PLoS One. 2016; 11(5):e0155808. doi: 10.1371/journal.pone.0155808. [CrossRef] [PubMed] [PMC free article]
- Crispim JN, Boto LR, Melo IS, et al. Acta Pediatr Port 2011:42(3):93-8. doi: 10.25754/pjp.2011.4226
- Owens J. Classification and Epidemiology of Childhood Sleep Disorders. Prim Care. 2008; 35(3):533-46, vii. doi: 10.1016/j.pop.2008.06.003. [CrossRef] [PubMed]
- McCoy JG, Strecker RE. The cognitive cost of sleep lost. Neurobiol Learn Mem. 2011; 96(4): 564-582. doi:10.1016/j.nlm.2011.07.004. [CrossRef] [PubMed] [PMC free article]
DOI: https://doi.org/10.7199/ped.oncall.2024.62
|
| Cite this article as: | | Andrade C, Câmara B, Freitas S, Freitas C, Sousa P. Characterization of Sleep Patterns and Disturbances in School-Aged Children: A Cross-Sectional Study in an Island Population. Pediatr Oncall J. 2024;21: 139-145. doi: 10.7199/ped.oncall.2024.62 |
|