Dr Ira Shah.
Medical Sciences Department, Pediatric Oncall, Mumbai, India. | | Case Report | A 2 month old male child born of third degree consanguineous marriage presented with loose motions since 3 days, vomiting since 1 day and aspiration of milk. The child was bottlefed with formula feeds. His antenatal and postnatal period was uneventful with a birth weight of 2.9 kg. Mother had no illness. He had achieved social smile at 2 months of age. He had an old sibling of 2 years age who was asymptomatic. On examination, he had coarse facies and extremities were cold though rectal temperature was normal. He had a dry and thick skin with a protruding tongue. Anterior fontanelle was wide-open 4 cm x 4 cm (Figure 1).
Figure 1: Congenital hypothyroidism


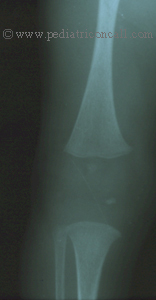
His anthropometry was still of neonatal proportions with length of 53 cm, weight of 3.5 kg and head circumference of 36.8 cm. There was no goiter on systemic examination, bowel sounds were absent and he was lethargic. There was no organomegaly. Deep tendon reflexes had delayed relaxation. Other examination findings were normal. He was diagnosed as sepsis with clinical suspicion of congenital hypothyroidism. Laboratory investigations revealed hemoglobin of 6.9 gm%, white cell count of 12,600 cells/cu mm with 70% polymorphs and 30% lymphocytes. His CRP was positive (2.4 mg/dl) suggestive of sepsis. He had metabolic acidosis with pH = 7.155 and bicarbonate of 12.3 mEq/L. Blood culture was negative. His thyroid profile was suggestive of hypothyroidism [T3 = < 0.2 ng/ml (Normal = 0.7 - 2 ng/ml), T4 < 1 mcg% (Normal = 5.5 to 13.5 mcg%) and TSH = 44 mcIU/ml (Normal = 0.2 to 5.1 mcIU/ml)]. USG of the thyroid showed no goiter and presence of thyroid gland with right lobe measuring 0.8 x 0.7 cms, left lobe measuring 0.8 x 0.7 cm and isthmus was 0.3 cm. A 2D Echo revealed mild pericardial effusion. His X-Ray of the lower limbs showed no tibial epiphysis [Figure 2].
Figure 2: Absent tibial epiphysis
Thus, he was diagnosed as congenital hypothyroidism most likely due to dyshormonogenesis with sepsis. A thyroid radionucleide scan has been advised and is awaited. He was treated with IV ceftriaxone and metronidazole. He was started on T. Thyroxin 50 mcg OD (13 mcg/kg/d) with folic acid supplementation. His clinical condition improved and child became more alert. Patient was discharged on T. Thyroxcin. | | | | Discussion | The prevalence of congenital hypothyroidism approximates 1 in 4000 birth.
Etiologies include:
- Thyroid dysgenesis (e.g. Aplasia, hypoplasia, ectopic thyroid) (75%)
- Thyroid dyshormonogenesis (TSH unresponsiveness, iodide trapping defect organification defect, defect in thyroglobulin) (10%)
- Hypothalamic-pituitary (TSH) deficiency (5%)
- Transient hypothyroidism (iodine, drug or maternal antibody induced) (10%).
Clinical Manifestations:
Congenital hypothyroid child may present with slightly increased head size due to myxedema of the brain. There may be prolongation of physiological jaundice, lethargy, somnolence, large tongue and nasal obstruction. Affected infants cry little, sleep more and are very lethargic. There may be presence of umbilical hernia, hypothermia, constipation, edema of genitals and extremities, cardiomegaly, bradycardia and asymptomatic pericardial effusion.
Symptoms appear gradually and if neonatal screening is not done, the diagnosis is often delayed. Ideally a neonatal screening (TSH screening) for CH should be routinely done in all children as treatment of affected infants within 45 days of birth leads to normal mental development. The TSH should be done 3 to 5 days after birth and patients with TSH levels more than 20-25 mU/L should be assessed further.
When there is partial deficiency of thyroid hormone as in ectopic thyroid and thyroid dyshormonogenesis, the symptoms may be milder. As the child grows, infantile proportions are maintained and child may have disproportionate short stature. Both anterior and posterior fontanelles are wide-open and coarse facies such as hypertelorism, depressed nasal bridge, puffiness of eyes; open mouth and short neck develop. Skin may appear yellow due to carotenemia. Hairline reaches far down on forehead and development is retarded. Voice is hoarse and child has hypotonia. Goiter may be seen in patients with dyshormonogenesis, thyroid hormone resistance and transient hypothyroidism.
Diagnosis:
Once clinically suspected or a positive neonatal screening test; the diagnosis is confirmed by serum T4 and TSH levels. The TSH will be elevated (>10 mcU/ml) and T4 will be low (<6.5 mcg/dl) in neonatal period in patients with CH. 20% of the infants may have normal T4 with modest TSH elevations. Such infants may require repeat examinations to establish a diagnosis of CH. Intrauterine deprivation of thyroid hormone may retard osseous centers and manifest as absent distal femoral epiphysis at birth.
APPROACH TO CONGENITAL HYPOTHYROIDISM

[Modified from:- Pediatric Endocrinology - Sperling MA, 1 st ed. Philadelphia, W.B. Saunders Company, 1996, pg 62.]
Treatment
Treatment should be started as soon as diagnosis is confirmed. The goal of therapy is early, adequate thyroid hormone replacement. It is desirable to maintain the serum T4 in the upper half of normal range in infants. An initial dose of thyroxine at 10-15 mcg/kg/day is recommended to minimize IQ loss. Infants with transient hypothyroidism should not be treated unless low T4 and elevated TSH persist beyond 2 weeks. Therapy in them should be discontinued after 8 to 12 weeks (in patients with maternal goitrogenic drugs) or by 5 months (in infants with maternal autoantibody).
T4 and TSH should be monitored at regular intervals. Overtreatment should be prevented and can be recognized by signs such as tachycardia, excessive nervousness, disturbed sleep pattern, advanced bone age and craniosynostosis.
Children may require a dose of 4 mcg/kg/day. | | | | Compliance with Ethical Standards | | Funding None | | | | Conflict of Interest None | | |
- Pediatric Endocrinology - Sperling MA, 1 st ed. Philadelphia, W.B. Saunders Company, 1996, pg 57-64.
- Nelson's Textbook of Pediatrics - Behrman RE et al, 16 th ed. Vol.2, Philadelphia, W.B. Saunders Company, 2000, pg 1698-1703.
|
| Cite this article as: | | Shah I. CONGENITAL HYPOTHYROIDISM. Pediatr Oncall J. 2004;1. |
|